Your Gum Health Explained, Part 1: Gingivitis
Do you get bleeding gums when you use dental floss? What about when you brush your teeth? Just sometimes? Or all the time?
All of us have probably had bleeding gums at some stage. If your gums get inflamed or bleed a little only once or twice a year, it may not be anything to worry about. But when it happens often and for a long time, then we need to find out why.
Why do our gums bleed? And what does it mean for your health? Are there different types of gum disease? Is it bad if we just leave it? We’ll find out the answers to these questions and more as we explore gum disease in this blog.
Gum Disease
Diseases of the gums, also known as periodontal diseases are possibly the most common diseases known to mankind. There are two main types:
- Gingivitis: which is chronic inflammation limited to the gums and is reversible
- Periodontitis: which is the next stage of gum disease and if left untreated, is irreversible and can lead to tooth loss.
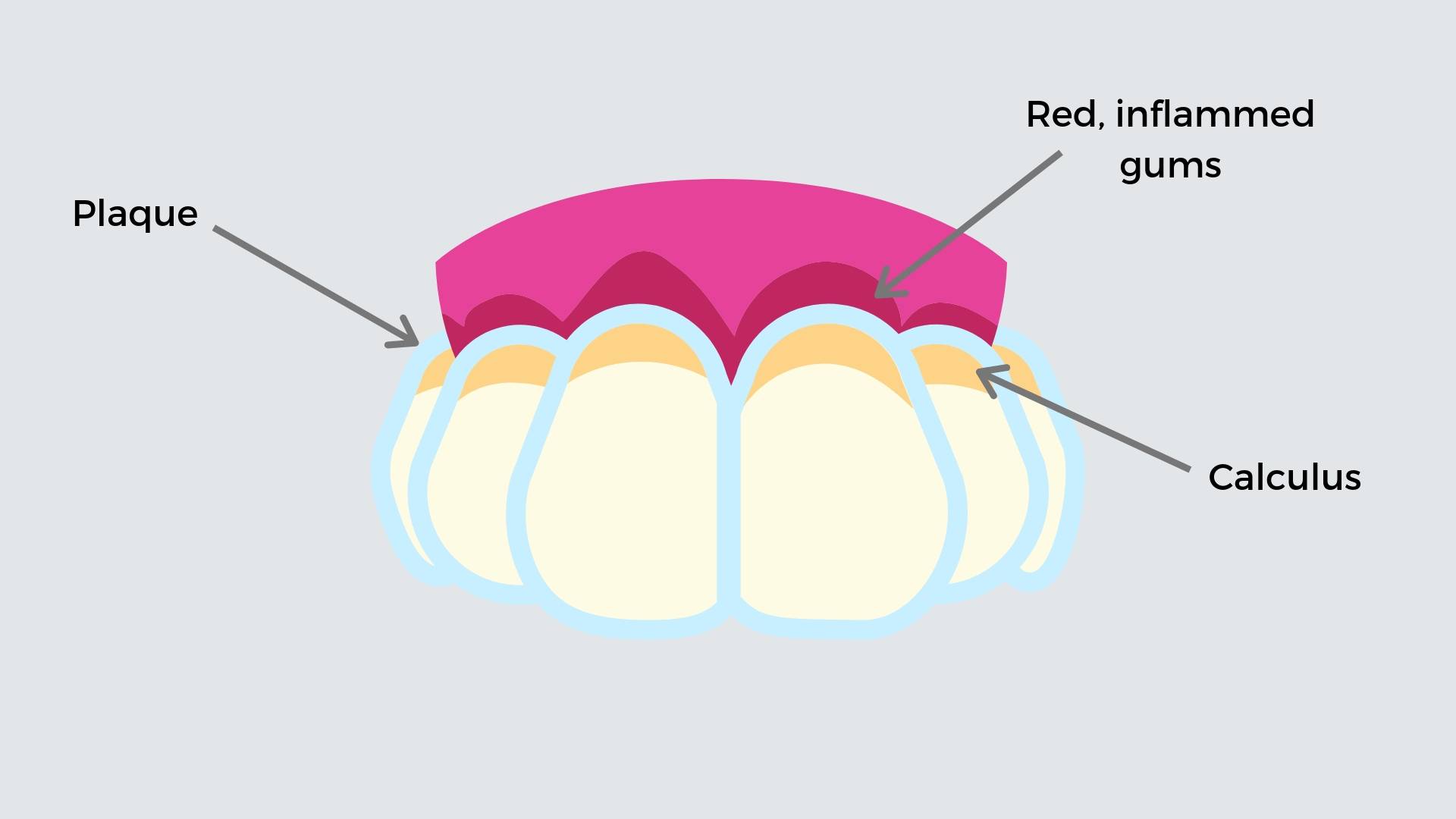
Gum diseases like these ones, are commonly caused by a buildup of plaque & calculus on our teeth along the gum line.

What is plaque and calculus?
Plaque is a colourless, sticky film made up of invisible masses of harmful bacteria. Some of these bacteria cause tooth decay, and then there’s different types of germs that cause gum disease. It forms all day, every day from eating and drinking as the germs multiply in your mouth. You are removing plaque every day when you brush and floss your teeth.
Calculus is hardened calcium deposits and dead germs stuck on your teeth, like barnacles on a boat, can be white or stained dark, and you can’t clean it off by yourself. When plaque builds up around the gums, and isn’t cleaned off, it hardens over time. With the help of calcium deposits from our saliva, this plaque turns into calculus.
What happens then?
Because calculus is rougher than tooth enamel, even more plaque grabs onto the calculus. Once there is new plaque on the calculus, it makes it super difficult for you to brush off. Day by day, more plaque builds up and hardens over time and well… you get the idea.
At the end of the day, your body can only tolerate so much. After a certain amount of buildup, your gums get annoyed and throws a hissy fit. Your immune system kicks in with an inflammatory response that tries to attack the germs in the plaque. This leads to redness, swelling and bleeding gums around the tooth. This early stage of gum disease is known as gingivitis.
So you can see, if plaque & calculus is left to fester on our teeth for long enough (ie if you don’t brush your teeth twice a day and visit the dentist regularly), it can cause some serious trouble, whether it be cavities or gum problems.
What does gingivitis do to me?
If your gums are inflamed, red or tender and bleed, even with regular brushing, it means that there’s a significant build up of plaque around your gum line. Bleeding gums is a signal; your immune system telling you to “Get it together!” This is a sign you need to up your oral hygiene game by brushing twice a day, flossing every day and visiting your dentist for a professional scale and polish. Find out more about proper brushing and flossing techniques here.

Should I be worried?
In the early stages of gingivitis, your gums may be irritated but the teeth are still firmly planted in their sockets. The inflammation is reversible and no major damage has been done to the tissues and bone that surrounds the teeth.
The problem comes when gingivitis isn’t stopped in its tracks. If it continues for long enough then it may progress to become Periodontitis. And you don’t want Periodontitis… We’ll have a blog about this up and ready soon so check back on 7th June 2019.
This is why it’s so important to visit your dentist for a full check-up and clean every 6-12 months (depending on your risk for tooth decay and gum disease). That way, your dentist can remove all of that nasty plaque and calculus that’s above or below your gum line where your toothbrush can’t reach.
And keeping your gums and teeth as healthy as possible is our mission here at Method Dental! You can find out more about what to expect on Your First Visit at Method Dental here

What increases my risk of developing gingivitis?
The most common cause of gingivitis is oral hygiene habits that aren’t quite up to scratch. But, there are also other lifestyle choices, medical conditions and medications that increases your risk of developing gingivitis. They include:
- Smoking or chewing tobacco
- Old age
- Dry mouth
- Poor nutrition, including vitamin C deficiency
- Poor quality fillings, crowns and bridge that make cleaning difficult
- Crooked teeth which also makes keeping surfaces in between the teeth and around the gum line difficult
- Conditions that compromise your immune system e.g leukemia, HIV/AIDS or cancer treatment
- Certain drugs, such as phenytoin for epileptic seizures, and some calcium channel blockers, used for high blood pressure and other conditions causes the gums to overgrow
- Hormonal changes e.g pregnancy, menstrual cycle
- Genetics
- Medical conditions such as certain viral and fungal infections
How is gingivitis treated?
We have some good news! With good oral hygiene habits and regular visits to the dentist, your gingivitis will get better!
Some people think they had better stop brushing your teeth and gums when you get bleeding gums. But you’ve got to keep on brushing as this will get rid of the bacteria and plaque that are causing the problem!
How can I prevent gingivitis?
Gingivitis can be prevented when proper plaque control is practiced. This means brushing for 2 minutes twice a day, flossing daily and most definitely, visiting your dentist for a professional scale and clean when advised. This will ensure your gums and teeth are always strong and healthy. And if there are nasties that pop up, at least it can be treated right away.

What happens if I ignore it? Out of sight, out of mind?
Unfortunately, untreated gingivitis can progress to become periodontitis, which is the advanced stage of gum disease. When this happens, your immune system goes into overdrive and ends up destroying the gums, ligaments and bone that hold the teeth in place.
Now, it’s no longer something that can be reversed. If your gum disease progresses to this stage, you’ll be at a much higher risk of developing painful infections, higher risks of conditions like heart disease and diabetes and you can even lose your teeth!
In our next blog, we’ll explore everything you need to know about periodontitis and what you can do before it’s too late.
Dr. Grant McGrath BDSc
Co-Founder, Principal Dentist
Method Dental
Jasmine Ooi BPharm
Co-Founder
Method Dental



